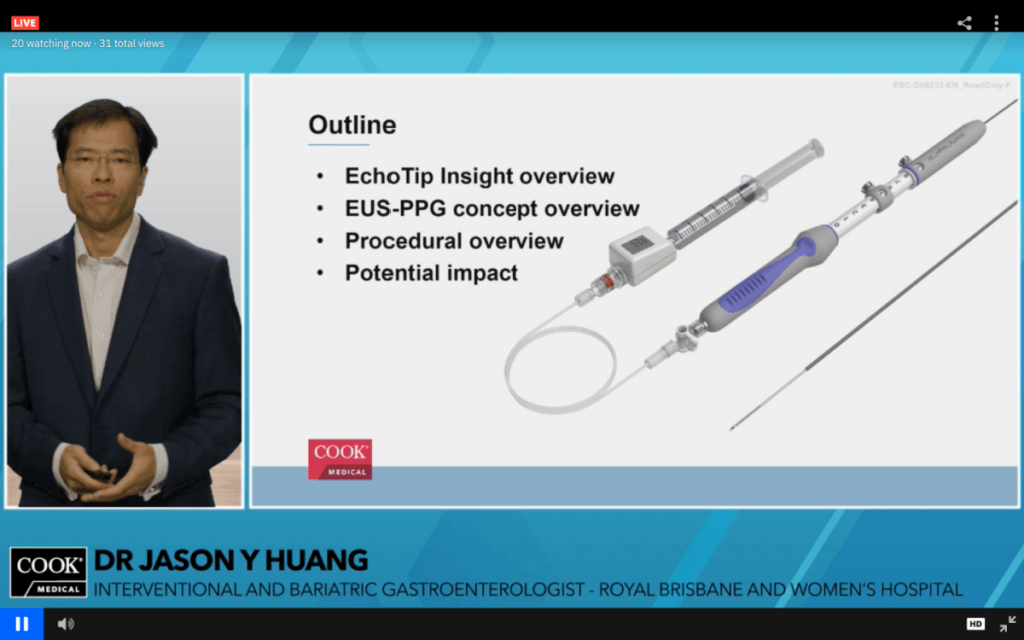
Dr Jason Huang, gastroenterologist from the Royal Brisbane Hospital, introduced the novel EUS-PPGM technique, performed using EchoTip Insight.
Brisbane, Australia. — At the virtual Endoscopic Ultrasound (EUS)-Guided Portosystemic Pressure Gradient Vista training held on 13 March 2021, Dr Jason Huang, a gastroenterologist from the Royal Brisbane Hospital, Brisbane, and Dr Avik Majumdar, a gastroenterologist and hepatologist from Royal Prince Alfred Hospital, Sydney, were invited to deliver lectures and case presentations based on their expertise and research efforts on the assessment and management of portal hypertension. Selected endoscopists and hepatologists from Australia, New Zealand and Hong Kong joined the training.
The hepatic venous pressure gradient (HVPG) accurately reflects the degree of portal hypertension and is widely considered the single best prognostic factor in liver disease. HVPG is a predictor of clinical decompensation in patients with compensated cirrhosis,1 an independent predictor of hepatocellular carcinoma development,2 and ‘has an independent effect on survival’ in patients with cirrhosis.3 Currently, HVPG is obtained through the standard transjugular approach, in which the portal vein pressure is indirectly estimated instead of directly measured.
The simple, novel EUS-guided portal pressure gradient measurement (PPGM) technique, introduced by Dr Huang in his lecture, allows for a direct portal vein pressure measurement, and therefore a direct PPG measurement. This method has demonstrated excellent correlation with pressure values obtained by the standard transjugular approach.4 The EUS-PPGM technique is performed with the EchoTip Insight™ Portosystemic Pressure Gradient Measurement System.
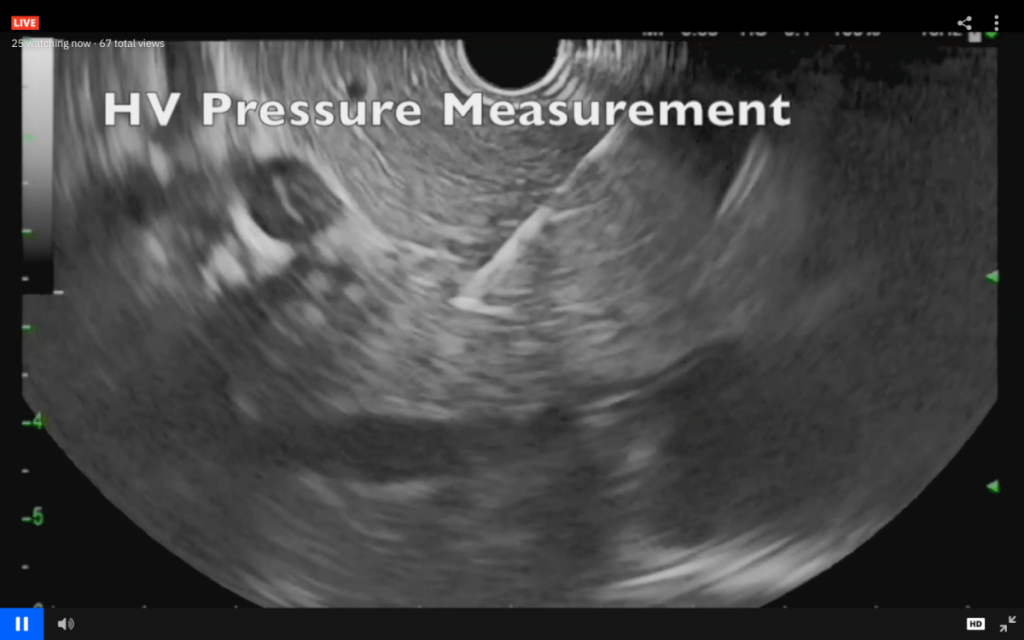
EUS image in which the EchoTip Insight, with its 25 gauge needle, directly accesses the hepatic vein for pressure measurement.
The EchoTip Insight was introduced to Australia in October 2020. Endoscopists can now support the new procedure to perform direct measurement of the portal and hepatic vein pressures under EUS guidance, so as to determine the appropriate treatment pathway for patients with liver disease. The procedure is less invasive and allows for comprehensive liver assessment through an endoscopic approach.
Dr Huang also provided reviews of the first human pilot study of EUS-PPGM in patients with liver disease. Key highlights of the pilot study include the following:
- The ‘novel technique of EUS-PPGM’ using the EchoTip Insight (which involves a 25-gauge needle and compact manometer) ‘is feasible and appears safe’.5
- ‘Twenty-eight patients underwent EUS-PPGM with 100% technical success and no adverse events.’5
- EUS-PPG values showed ‘excellent correlation with clinical parameters of portal hypertension’.5
- ‘Given the availability of EUS and the simplicity of the manometry setup, EUS-guided PPG may represent a promising breakthrough for procuring indispensable information in the management of patients with liver disease.’5
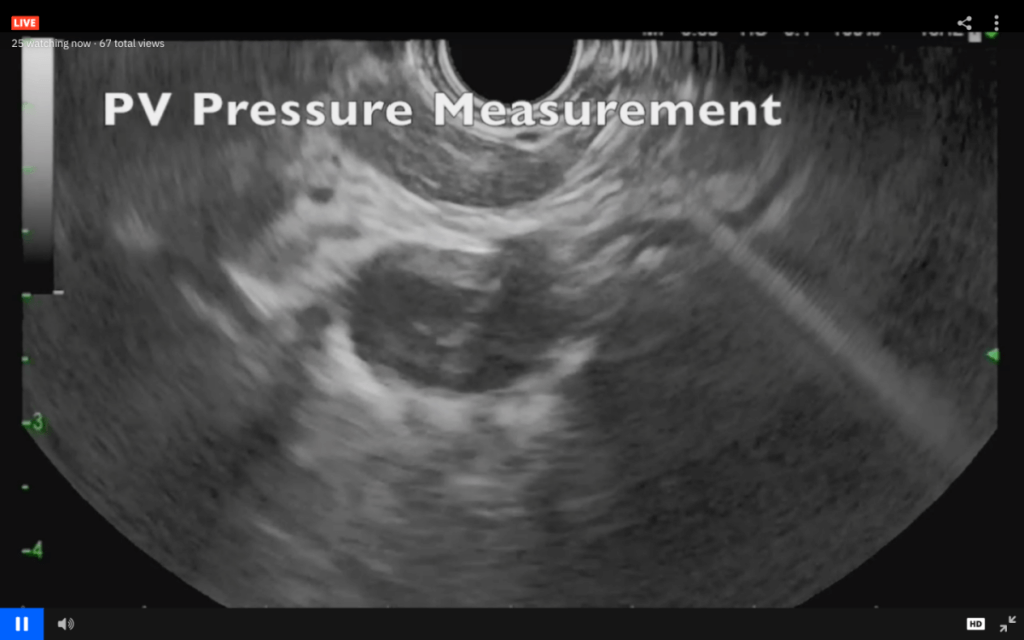
EUS image in which the EchoTip Insight, with its 25 gauge needle, directly accesses the portal vein for pressure measurement.
Dr Avik Majumdar started his session by providing a review of both invasive and non-invasive diagnostic procedures for different clinical stages of liver diseases. He explained the basis of portal hypertension, the clinical applications of HVPG, the setup of HVPG procedures and their potential limitations in that they require access to an angiography suite.
In the concluding session, Dr Majumdar emphasised the need for providing personalised treatment to patients according to their portal pressure measurements and the ideal of offering ‘one-stop’ solutions for diagnosis, prognosis and therapy for portal hypertensive patients.
Participants actively asked questions during the training, and Dr Huang and Dr Majumdar provided answers. Some of the exchanges between the participants and the presenters include the following:
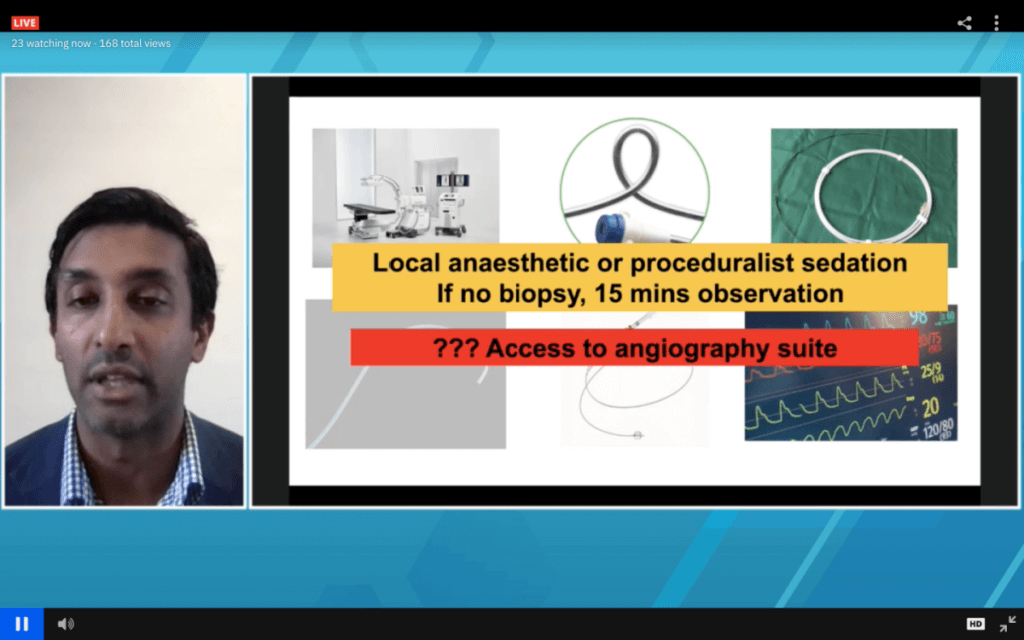
Dr Avik Majumdar, gastroenterologist and hepatologist from Royal Prince Alfred Hospital, addressed the participants with an insightful lecture on portal hypertension and HVPG applications.
- How long does it take to perform the EUS-PPGM procedure?
- Usually between 15 and 30 minutes, depending on how quickly the landmarks are identified in the procedure.
- What does the learning curve look like in this procedure?
- It depends on the physician’s understanding of the liver anatomy and also their ability to identify the targeted blood vessels.
- Is the presence of large varices a contraindication?
- It depends on the liver anatomy of the patient and whether the physician is able to find an access window; based on Dr Huang’s and Dr Majumdar’s initial experiences, this is not a problem.
- Are there any types of patients for whom you think EUS-PPG would be feasible but not HVPG?
- Post-liver transplant patients and post-liver resection patients, since accessing the hepatic vein would be difficult.
For more information on our Vista trainings or EchoTip Insight, you may contact us online or contact your local Cook representative.
About Cook Medical
Since 1963, Cook Medical has worked closely with physicians to develop technologies that eliminate the need for open surgery. Today we invent, manufacture and deliver a unique portfolio of medical devices to the healthcare systems of the world. Serving patients is a privilege and we demand the highest standards of quality ethics and service. We have remained family owned so that we have the freedom to focus on what we care about: our patients, our employees, and our communities.
Cook Medical Australia has more than 600 employees in manufacturing, distribution, engineering and technical specialties. The company exports more than 90% of its locally manufactured products to medical providers worldwide with devices across two product families: endovascular grafts for the treatment of vascular disease and in vitro fertilisation to assist those trying to conceive a child.
For more information, please visit www.cookmedical.com.au and like us on Facebook, and LinkedIn.
References:
- Ripoll C, Groszmann R, Garcia-Tsao G, et al. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Gastroenterol. 2007;133(2):481–488.
- Ripoll C, Groszmann RJ, Garcia-Tsao G, et al. Hepatic venous pressure gradient predicts development of hepatocellular carcinoma independently of severity of cirrhosis. J Hepatol. 2009;50(5):923–928.
- Ripoll C, Bañares R, Rincón D, et al. Influence of hepatic venous pressure gradient on the prediction of survival of patients with cirrhosis in the MELD era. Hepatology. 2005;42(4):793–801.
- Huang JY, Samarasena JB, Tsujino T, et al. EUS-guided portal pressure gradient measurement with a novel 25-gauge needle device versus standard transjugular approach: a comparison animal study. Gastrointest Endosc. 2016;84(2):358–362.
- Huang JY, Samarasena JB, Tsujino T, et al. EUS-guided portal pressure gradient measurement with a simple novel device: a human pilot study. Gastrointest Endosc. 2017;85(5):996–1001.